Radioactive Substances Help Produce Better Images
Cancers of the esophagus have been linked to alcohol and tobacco use, and excess body weight. They also come with a relatively high mortality rate. However, survival rates for people with early stage cancer are higher, making early and accurate diagnosis vital.
Main Street Radiology uses several types of advanced medical technology to diagnose and monitor the disease. These include endoscopic ultrasounds, which involve threading a flexible tube carrying a small camera into the patient's esophagus. We also use esophagrams, which are X-rays taken after a patient swallows a radioactive liquid containing barium. Lastly, there is positron emission tomography (PET), a scan that also makes use of a radioactive tracer to produce detailed images of the esophagus and any tumors or masses.
Case History: A 51-year-old male had a biopsy which revealed adenocarcinoma of the esophagus. The patient was referred to Main Street Radiology for an esophagram and whole-body PET scan.
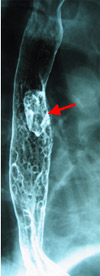
Figure 1

Figure 2

Figure 3
Findings: The air contrast esophagram (Figure 1) demonstrates a polypoid mass (arrow) in the mid-esophagus, compatible with carcinoma. Nodular changes of the distal esophagus may represent superficial spread of malignancy, esophagitis, or Barrett esophagus.
Coronal (Figure 2) and sagittal (Figure 3) PET images show a single hypermetabolic focus in the mid-esophagus corresponding to the mass seen on the esophagram. Normal activity is present within the distal esophagus, indicating absence of malignancy. No distant metastases are evident on the PET scan.
Discussion: Barrett esophagus represents replacement of squamous epithelium of the esophagus by metaplastic columnar epithelium, secondary to chronic gastroesophageal reflux. These patients have a 40-fold higher risk than the general population in developing adenocarcinoma. Squamous cell carcinoma typically represents greater than 90% of esophageal cancers.
Accurate staging is crucial in patients with esophageal cancer, due to the poor prognosis and risks involved with extensive surgery. PET has been shown to be the most accurate non-invasive imaging modality in detecting distant metastases (Am J Roentgenol 1997; 168:417-424), superior to CT. Although not advocated for use in screening, PET has also achieved nearly 100% sensitivity in detection of the primary tumor in patients with known esophageal cancer. Neither CT nor PET has shown the accuracy of endoscopic ultrasound in detecting local invasion. Therefore, pre-operative staging of esophageal cancer should include both PET and endoscopic ultrasound. In addition, PET is advocated as the most accurate imaging study to detect recurrent disease, and to follow patients who have undergone chemotherapy and radiation therapy (Radiographics 2000;20:713-723).
Esophageal cancer, including squamous and adenocarcinoma, is one of many oncological indications approved for reimbursement by Medicare/Medicaid and most private insurance companies.